The Centers for Advanced Orthopaedics is redefining the way musculoskeletal care is delivered across the region with locations throughout Maryland, DC, Virginia and Pennsylvania.
Spinal Compression Fractures
Back pain is an extremely common problem, especially as we get older. So how do you know when it may be something more serious?
If you are over the age of 50 or have been diagnosed with a condition that causes bone weakening—such as osteoporosis or cancer—back pain may be a sign of a spinal fracture.
According to the American Association of Neurological Sciences, roughly 750,000 individuals each year are diagnosed with vertebral compression fractures. These spinal fractures are especially common in patients with weakened bones; however, fractures can also occur in healthy spines due to severe trauma—such as a sports injury or car accident.

What is a Compression Fracture of the Spine?
The spine consists of 33 bony blocks, called vertebrae, which are stacked on top of one another. Small cracks in the vertebrae can occur and spread over time, leading to a complete vertebral fracture. If left untreated, the fractured vertebra can eventually collapse causing pain, limited mobility, and deformity.
These fractures are most common in the thoracic spine, which is below the upper body and centered in the middle of the back. Most compression fractures occur towards the front of the vertebra, as the back of the spine is made up of harder bone and less prone to injury.

How Do Spinal Compression Fractures Happen?
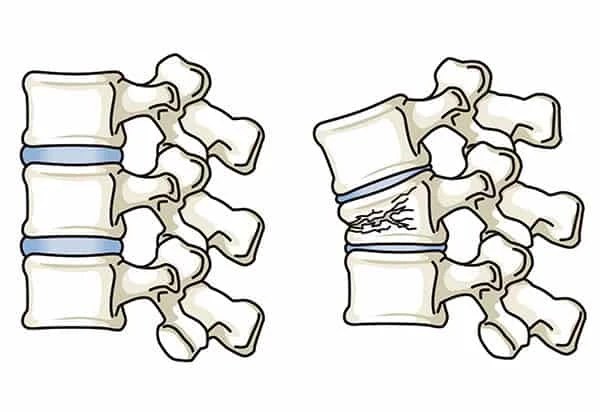 Vertebral compression fractures are typically the result of osteoporosis. Over time, the vertebral discs dry out and lose strength while the bone of the vertebrae becomes porous and brittle. The concurrent weakening of these structures leaves the spine vulnerable to injury as the spinal vertebrae are not strong enough to carry the weight of everyday events. These “everyday events” can range from lifting an object to something as simple as sneezing or coughing.
Vertebral compression fractures are typically the result of osteoporosis. Over time, the vertebral discs dry out and lose strength while the bone of the vertebrae becomes porous and brittle. The concurrent weakening of these structures leaves the spine vulnerable to injury as the spinal vertebrae are not strong enough to carry the weight of everyday events. These “everyday events” can range from lifting an object to something as simple as sneezing or coughing.
Symptoms of a Spinal Compression Fracture
Common symptoms of a spinal compression fracture include:
Back pain that has a sudden onset. Pain may intensify when walking or standing and decrease when lying down.
Loss of height. After a number of compression fractures, the shape of the spine can change. Height loss can occur as the spine compresses and becomes shorter.
Dowager’s Hump. Also called kyphosis, dowager's hump occurs when the back of the vertebra remains stable while the front portion erodes. This causes a wedge-like curvature of the spine leading to a stooped posture.
Risk Factors for Spinal Compression Fractures
As we age, the likelihood of developing this condition rises, especially among women due to increased risk for osteoporosis. According to AANS, approximately 25% of postmenopausal women are affected by spinal compression fractures with 40% of women over the age of 80 affected.
However, while women are more susceptible to spinal fractures, they are an important health concern for older men as well.
There are two main risk factors for compression fractures of the spine:
Osteoporosis is the most common risk factor for spinal compression fractures. Risk factors of osteoporosis include:
- Race. White and Asian women are at a higher risk for osteoporosis due to a genetic predisposition.
- Age. Women over the age of 50 are at a higher risk.
- Weight. Slim women are more likely to develop osteoporosis due to fragile bone structure.
- Early menopause. Women who experience menopause before the age of 50 are at risk for osteoporosis.
- Smoking is known to be connected to a loss in bone thickness.
Cancer that has spread to the bones can also put you at risk for compression fractures. Certain types of cancer are monitored for spinal fractures—myeloma and lymphoma being the most common. However, in some cases, a fracture can be the first sign of cancer.
Following a spinal compression fracture, the risk of future fractures greatly increases, even if symptoms are minor. If you suspect a spinal fracture, it’s important to see a doctor to prevent potential spinal deformity.
Diagnosis & Treatment
Methods of Diagnosis
 If a spinal compression fracture is suspected, there are a number of ways a diagnosis can be reached.
If a spinal compression fracture is suspected, there are a number of ways a diagnosis can be reached.
Typically, this process will begin with a physical exam. The exam will include questions regarding symptoms, performing certain movements to gauge pain, and feeling for tenderness in the vertebral body near the spinal cord.
Following a physical exam, further scans may be ordered to provide a more detailed view of the area. These scans can help to confirm a diagnosis as well as predict prognosis to determine the best course of treatment.
Common scans include:
An X-ray is used to take a picture of the bones in the spine. This may be used to outline the joints and take note of the structure of the vertebrae. Any abnormalities in bone alignment, disc degeneration, or bone spurs in the spinal cord or nerves can be identified.
A CAT or CT scan can help determine the shape and size of the spinal canal and the structures surrounding it. A myelogram may also be completed with a CAT or CT scan. This includes a spinal tap where a dye is inserted into the spine to increase detail in the produced images.
An MRI scan forms a three-dimensional image of the back. With this scan, the nerve roots, spinal cord, and possible tumors can be identified and examined. An MRI is mainly used to provide detailed images of the soft tissues in the surrounding area.
A bone density test is used to measure calcium and other minerals in the bones and is the most accurate way to determine if osteoporosis is present in the spine. Small changes in the bone mass can also be determined.
Treatment Options
If a spinal compression fracture is confirmed, immediate treatment is essential in reducing the risk of further damage. There are a variety of treatment options available depending on the cause and severity of the condition.
Non-Surgical Treatment
Pain medications. Non-steroidal inflammatory drugs such as Aleve (naproxen sodium) or ibuprofen can aid in reducing pain. Muscle relaxants may also be prescribed.
A back brace can be used to provide spinal stability and limit any sudden or extreme motion in the spinal area. The extra stability and lack of movement may also aid in reducing pain.
If non-surgical treatment is ineffective or damage is more severe, spine surgery may be recommended.
Surgical Treatment
There are two main types of surgeries available, both are minimally invasive. They are as follows:
Vertebroplasty. Vertebroplasty typically takes one to two hours to complete and is often done on an outpatient basis. During this procedure, a needle containing acrylic bone cement is injected into the vertebra to stabilize fracture(s).
Kyphoplasty. A similar procedure to vertebroplasty, this technique involves the use of a balloon to guide the cement and straighten the bone. The balloon makes space in the spine for the cement to be placed.
Spinal compression fractures can occur gradually over time and, if left untreated, can have long-lasting effects. Aging doesn't necessarily mean that aches and pains should be a part of everyday life. We are here to help guide you on the path to recovery.
OrthoMaryland’s extensively trained orthopedic spine specialists provide the latest in both surgical and nonsurgical treatment options for back pain and conditions affecting the spine. Members of our spine team evaluate each case carefully to maximize patient satisfaction and recovery. Contact us today to learn how we can help you!
Request an Appointment
-
 Physical Medicine and Rehabilitation – Traditional and Interventional
Physical Medicine and Rehabilitation – Traditional and Interventional -
 Physical Medicine and Rehabilitation – Traditional and Interventional
Physical Medicine and Rehabilitation – Traditional and Interventional