The Centers for Advanced Orthopaedics is redefining the way musculoskeletal care is delivered across the region with locations throughout Maryland, DC, Virginia and Pennsylvania.
Osteoporosis and the Spine
 According to the National Osteoporosis Foundation, osteoporosis affects more than 54 million Americans and is responsible for over 2 million broken bones a year. These staggering statistics continue to increase with each passing year.
According to the National Osteoporosis Foundation, osteoporosis affects more than 54 million Americans and is responsible for over 2 million broken bones a year. These staggering statistics continue to increase with each passing year.
Osteoporosis is most commonly found in women over the age of 50 and in men over the age of 70. In fact, 1 in 2 women (50%) and 1 in 4 men (25%) will experience an osteoporosis-related fracture in their lifetime.
What is Osteoporosis?
The term osteoporosis—translated from the Greek language meaning “porous bone”—refers to a degenerative condition that causes bones to lose their density and strength. As we grow older, this condition leads to our bones becoming very weak and increases the risk for breaks and fractures.
While most of the tissue in the human body uses cell division to grow, heal and repair itself, our bones use a different process to achieve this, called bone remodeling. The body is continually breaking down old bone cells and extracting calcium and phosphorous which is then reintroduced into the bloodstream in a process known as resorption. Through the remodeling process, the body is able to use these minerals to help replenish the old bone cells with new bone cells.
When we are young, our bodies produce bone cells faster than it is able to break them down which is essential to increasing our body’s bone mass structure. As we age, that rate begins to flatten out. Generally, we reach peak bone mass between the ages of 18 and 25; this is where the rate of resorption and remodeling are equal. When the body breaks down old bone cells faster than it is able to replenish them, the bones become weak and susceptible to breaks or fractures. This is known as Osteoporosis.
How Does Osteoporosis Affect the Spine?
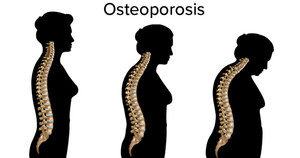
The spine is made up of a series of vertebrae which are stacked on top of one another. As osteoporosis sets in and bone loss begins to occur, the vertebrae become weak and brittle. When the spine is weakened by osteoporosis, it can be fractured by something as simple as a minor fall, lifting a heavy object, or even a cough or sneeze.
Symptoms of Spine Fractures
Spinal fractures are unlike fractures in the arm or leg, which typically cause a significant amount of immediate pain. Instead, when a fracture occurs in the spine, the vertebrae collapse and compress, often without causing any pain at all. Over time, symptoms may worsen and can include:
- Height loss
- Back pain
- Trouble bending or twisting
- Spinal deformities—such as a stooped, curved posture called Kyphosis (also known as “Dowager's Hump”).
How is Osteoporosis Diagnosed?
Since the effects of osteoporosis occur gradually, it can be difficult to diagnose. Early detection of osteoporosis is carried out by screening risk factors based on age and sex.
Generally, all women over the age of 65 and postmenopausal women with qualifying risk factors need to be screened for low bone density. There is a direct connection between the development of osteoporosis and lack of estrogen production caused by menopause. Therefore, it is widely recommended that women see a physician about getting screened as early as age 50.
Men are at less risk of developing osteoporosis; therefore, there is no official recommendation for screening. It is generally advised that men over the age of 70 should be screened for osteoporosis.
How Can I Protect My Spine?
Proper movement is essential in protecting the spine from excess stress and injury. The National Osteoporosis Foundation offers these recommendations:
- Do not bend or twist from the waist or trunk
- Do not lift or carry heavy objects
- Do not bend forward when coughing or sneezing
- Do not reach for objects up high
- Do not do toe-touches, sit-ups, or crunches
Unfortunately, there is no cure for osteoporosis, however, there are preventative measures that can significantly minimize risk and help improve quality of life for those living with osteoporosis.
- Quit Smoking. Smoking causes levels of hormones to decrease which slows down bone growth.
- Limit Alcohol Usage. Limiting alcohol usage minimizes accidental falls and slips helping to preserve your bone’s health.
- Exercise. Having a regular exercise routine, such as walking, weightlifting, bicycling, swimming, etc. can help strengthen the muscles that help support your bones.
- Yoga. Yoga helps to keep your body flexible and improves balance, reducing your chances of accidental falls and fractures.
- Vitamin D and Calcium. These are essential for bone growth. Make sure to ask your physician for the proper dietary intake of each.
Awareness and prevention are the key to ensuring that osteoporosis doesn’t take control of your life. Start taking matters into your own hands. Consult your doctor today to see if you may need to schedule an osteoporosis screening. Should you encounter back pain, a spine specialist—such as a Physical Medicine & Rehabilitation specialist, PM&R physician, or Orthopaedic spine surgeon—can offer you the best treatment options.